Dr. Christine Ren-Fielding: BMI Should Not Be Sole Measure of Obesity
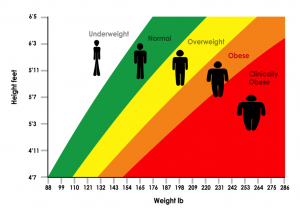
UncategorizedRecent research from the NYU School of Medicine has doctors reconsidering the standard practice of determining obesity using the Body Mass Index (BMI). Using the height and weight of a person, BMI is calculated to classify the patient as underweight, normal weight, overweight, or obese. Most people are familiar with seeing it represented as a number from about 15-40 with 18.5-25 considered “normal”. Another common representation of BMI is a chart where height and weight meet at the person’s BMI. But is height and weight the right way to measure BMI?
Dr. Christine Ren-Fielding Believes BMI Is Not Enough
While BMI is a decent snapshot, height and weight are not enough to classify something as important as whether or not a person is obese. The NYU School of Medicine research supports this. The study posits that height and weight alone are not good indicators of obesity because they do not look at other physiological factors. In fact, the report shows that when only BMI is used to determine whether or not someone is obese, nearly 40% of people can be classified incorrectly.
The study on a scaled, representative sample of 1400 patients used three tests:
- Two tests of leptin in the blood. Leptin regulates metabolism and measuring it can help determine obesity.
- Dual Energy X-Ray Absorptiometry (DXA). DXA measures bone density, body fat, and muscle mass.
Researchers found that when using these indicators and comparing them to the calculated BMI of subjects, the BMI was an average of 4 points lower for patients. 39% of subjects were thus improperly labeled as not obese when just BMI was used while the DXA showed that they were actually obese.
The limitations are amply clear and Dr. Christine Ren-Fielding is pleased that there is research that will help present a new opinion on the outdated use of BMI as the be all and end all of measuring obesity. Height and weight, while a good initial indicator, cannot take into account factors such as the loss of muscle mass which might result in someone being considered overweight when they are, in fact, obese. She is also pleased that the report highlights that these additional tests can be performed at a minimal cost.
The results of the NYU School of Medicine study reinforce and further Dr. Christine Ren-Fielding’s position that BMI is too relied upon as an indicator of obesity and to determine treatment and that the number is, essentially, arbitrary in light of the fact that there are three other simple tests that can give doctors and patients a more rounded view of their overall health and weight. Dr. Christine Ren-Fielding is encouraged by this shift in thinking and hopes that it will become the accepted way to assess obesity and allow more patients access to needed treatment. You can learn about the obesity treatment Dr. Christine Ren-Fielding offers at NYU Langone Weight Management or register to attend a free information session.
No comments yet.